March 23, 2025, Volume 2, Issue 1
Do the options for coding patient visits ever seem overwhelming? With multiple levels (1-5), different methods for determining levels (time vs decision making), and the ability to combine evaluation/management (E/M) visits with well-child care or procedures, using modifiers and proper documentation, coding can be complex. This issue will help clarify key points!
Quick improvements
1. Use definitive diagnoses instead of symptom codes when applicable.
Example: If a rapid strep test (RST) confirms Strep throat, do not include codes for fever and/or sore throat, as Strep throat is the final diagnosis
Our Compliance audits identified the following Top 5 best practices:
2. Ensure compliant vaccine counseling documentation.
Example: “I have performed vaccine counseling and answered all questions from the patient and parents(s) on risks and benefits for all vaccine components.”
3. Document time spent in your note when using time-based billing to justify visit level. The time clock you see in EPIC is not reported.
4. Use ‘Z100.121 Encounter for routine child health examination with abnormal findings’ when appropriate, instead of ‘Z100.129 for Encounter for routine child health examination without abnormal findings.’
Examples: patient has URI symptoms, a new heart murmur is detected, or the patient has exacerbation of a chronic condition.
5. Provide documentation that fully supports the level of service billed.
Documenting your VISIT Level
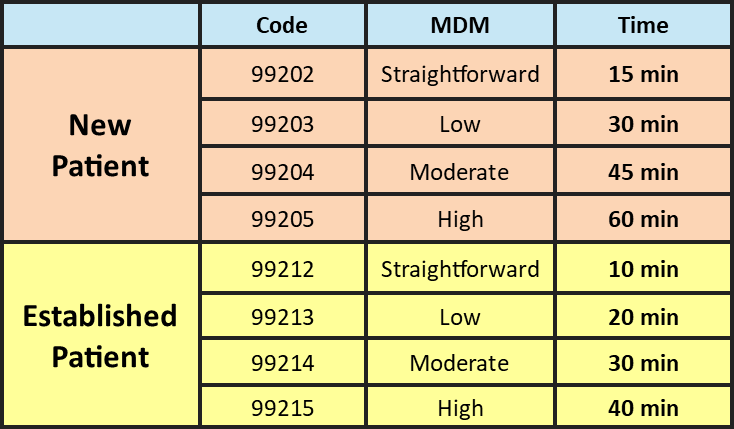
A visit level is determined either by Time or by Medical Decision Making (MDM). Documentation should support the chosen method and include a medically appropriate history and physical examination.
Essential Elements of Strong Documentation
Regardless of whether Time or MDM is used, documentation should:
· Identify suspected or confirmed primary diagnosis.
· Characterize pertinent ACTIVE & CHRONIC diagnoses.
· Demonstrate medical necessity.
· Outline the plan of care.
· Support reported professional codes.
Maximize Your Visit Leveling
· Choose MDM or Time strategically to your advantage.
· Time-based coding is most beneficial when total time spent exceeds the corresponding time requirement for MDM.
· Always document and code to the highest level of specificity to ensure accurate and appropriate reimbursement.
Medical Decision Making (MDM) Visit Leveling
The Medical Decision Making (MDM) level is determined by meeting two out of three key 3 element. These elements are:
1. Problems: Establishing Diagnoses & Severity
· Number & complexity of problems addressed during the encounter
· Include actively treated or considered issues.
· Include chronic condition when:
Þ Addressed as a problem.
Þ The condition increases risk or complicates the main problem.
· The pre-populated “Problem List” does not count toward MDM.
2. Data: Assessing Condition Status
· Amount and/or complexity of data reviewed and analyzed.
· Each unique test, order, or document contributes to the combination of 2 or 3, based on the level.
· Your interpretation of a test.
Þ Document: “I independently interpreted…”
Þ MAY NOT be separately reported elsewhere.
· YOUR discussion with other qualified professionals about the case.
3. Risk: Selecting Management Options:
· Risk of complications, morbidity and/or mortality based on patient management decisions made during the visit.
· Escalating or de-escalating the setting or level of care.
· Consideration for a high-risk plan of care.
· Document your decision-making process to support the level or risk.
Time-based Visit Leveling
Counted time occurs on the day of the visit and includes:
· Visit preparation
· Obtaining history
· Performing exam
· Caregiver counseling
· Orders
· Communications
· Documentation
· Interpreting results (not separately reported elsewhere)
· Care coordination (not separately reported elsewhere)
Activities not considered for time include:
· Documentation/review the day before the visit
· Documentation the day after the visit
· Clinical staff time
· Resident/fellow time
· General teaching
· Travel
Modifier –25
Modifier -25 should be appended to an E/M code when a significant, separately identifiable E/M service is performed on the same day of a procedure or other service by same physician. Common scenarios include:
• Preventative visit with a sick visit.
• E/M visit with a procedure.
• E/M visit with vaccinations.
• E/M visit with developmental/behavioral/caregiver screening.
Modifier –25 may only be appended to E/M codes. A single progress note may be used for all services, but documentation must clearly support each service as distinct.
Insignificant or trivial concerns encountered during another service (e.g., minor diaper rash, renewal of prescription medications, minor cold), which do not require additional work and performing the key components (history, physical, MDM/time) should not be reported separately.
Office Procedures
Many office procedures have reportable CPT codes, where evaluation elements performed before and after a procedure are considered inherent to the procedure, and should not be reported separately:
Abscess incision & drainage Urinary catheterization
Skin tag removal
Gastrostomy tube replacement
Chemical cauterization
Impacted cerumen removal
Laceration repair
Casting / splinting
Foreign body removal with incision
Injection / infusion
Certain minor procedures are not reported separately (i.e. nonimpacted cerumen removal, abscess puncture without aspiration, adhesive strip wound closure), coding based on time may be most appropriate.